What you need to know about SCOTUS, the Affordable Care Act and its effects on birth control access…
What you need to know about birth control in 2020:
- Get it before the ACA is reversed.
- You can get a year’s supply in some states.
- Get some prescription emergency contraception too!
- How you can help protect access to birth control.
- There’s a new ring, new patch, and new progestin-only pill.
If you have a uterus and are of reproductive age, you might want to consider getting an IUD or implant now. Why? Because on Nov 10th, the Supreme Court of the US (SCOTUS) began hearing arguments in California v. Texas, which could end up with the ACA (Affordable Care Act) being rendered unconstitutional.
How does that relate to birth control access? Under the ACA, all FDA approved methods of birth control for those with uteri are required to be covered for “free,” meaning that there is no copay and no deductible. However, if the SCOTUS strikes down the ACA, then this could end.
The ACA birth control mandate has saved women and their families millions of dollars. It is estimated that in the first year the ACA birth control mandate was in effect, it saved women $1.4 billion. “The average pill user saved $254.91 per year.” Before the ACA, out-of-pocket expenses for birth control accounted for 30-44% of women’s out-of-pocket health care spending. After the ACA, women could spend that money on rent, food, etc. By increasing access to birth control, we decrease abortion and unplanned pregnancies, resulting in better economic opportunities and education for women and their families.
If you are on the birth control pill, patch, or ring, know that in 17 states you can get a year’s supply of birth control at a time, so consider getting as much birth control as you can now. By law, these states require insurances to provide a year’s supply of birth control pills at a time: California, Colorado, Connecticut, Delaware, Hawaii, Illinois, Maine, Maryland, Massachusetts, Nevada, New Hampshire, New York, Oregon, Rhode Island, Vermont, Virginia, and Washington. Contact your prescriber to write a year’s supply. Let your provider know “it’s the law” in your state. (You can ask for 13 or 17 packs of pills, 13 rings, or 39 or 52 patches.)
If you have any problems getting a year’s supply because your insurance refuses, call your insurance and say “it’s the law.” If that doesn’t work, then contact CoverHer.org, a project of the National Women’s Law Center. They have sample scripts to argue with your insurance companies and letters that you can write.

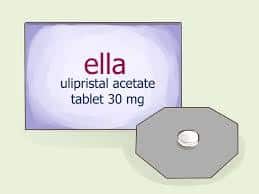
If you have a uterus and are of reproductive age, get some prescription emergency contraception now. Again, the ACA covers it with no copay and no deductible, so it’s “free.” Prescription emergency contraception (Ella) works better at every time point and for BMIs of 26-35 when compared to Plan B and its generics. If you have a BMI of 26 or greater, know that Plan B and its generics probably won’t work, so please CHECK your BMI.
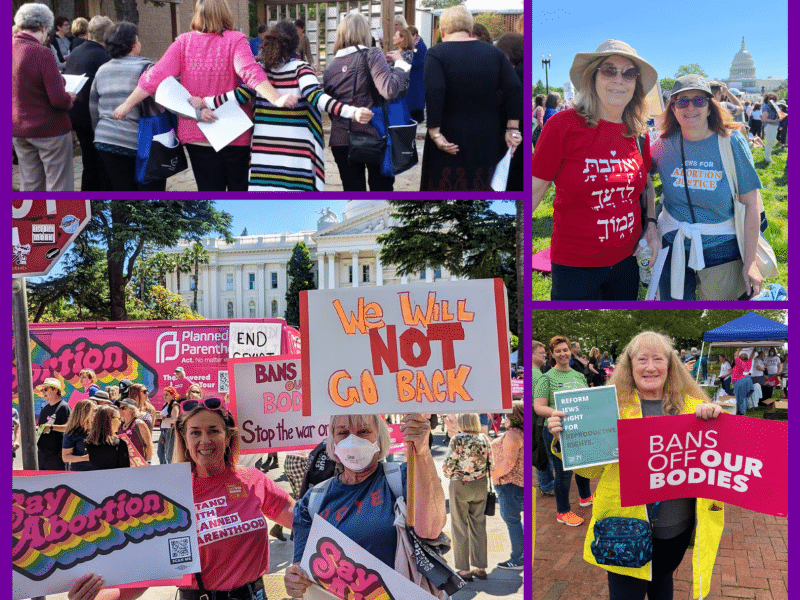
What can you do if you support those with uteri having access to “free” (no copay, no deductible) birth control?
Tell SCOTUS: #KeepTheACA #SaveTheACA. Chief Justice John Roberts is known to be receptive to public opinion and does not want to go down in history as a bad Chief Justice. So PROTEST, get on social media, and make it clear: The ACA benefits the public, and we want it to stay.
Tell insurance companies and State Government Officials: It is fiscally smart and morally right to cover birth control. So even if the ACA is overturned, there is nothing stopping insurance companies from providing birth control with no copay, no deductible, and there is nothing stopping politicians and elected officials from passing laws mandating coverage for “free.” It is far cheaper to cover birth control than to pay for an unplanned pregnancy. It costs $800 for an abortion, $10,000 for a vaginal delivery, and $40,000 for a C-section. That does NOT include the pre- and postnatal care, well-child visits, ultrasounds, lab tests, etc. For every $1 spent by the government on birth control, it saves $7 on healthcare expenses.
Kudos to the 29 states and Washington, D.C that mandate birth control coverage. Kudos to the 16 states and Washington, D.C. that have passed laws to keep the birth control mandate in place even if the ACA is reversed. Check for your state here.
Long-acting reversible contraception (LARC) and permanent contraception/sterilization is expensive but effective.
An IUD/implant could cost $1300, so get an IUD or implant NOW if you are considering it. If you are thinking about permanent contraception, a tubal ligation can cost up to $6000, whereas a vasectomy is only $1000 and far less invasive and more effective.
Per Contraceptive Technology 2018, the chart below provides statistics of the typical failure rates of these options:
| Failure Rate | Duration | |
| 19-20 mcg IUD with hormone (Liletta, Mirena) | 1/1000 | 5-7 yrs |
| Implant | 1/1000 | 3-5 yrs |
| Vasectomy * | 1.5/1000 | forever |
| 17.5 mcg IUD with hormone (Kyleena) | 2/1000 | 5 yrs |
| 14 mcg of IUD with hormone (Skyla) | 4/1000 | 3 yrs |
| Tubal Ligation | 5/1000 | forever |
| Copper IUD | 8/1000 | 10-12 yrs |
*Not covered by the ACA but covered by Illinois, Maryland, New Jersey, New Mexico, New York, Oregon, Vermont, Washington.
To learn more about these methods, click here.
The hormonal IUDs result in lighter (70% of users) or no periods (30%). The copper IUD causes more cramps and more blood loss but is a good option if you can’t use anything with hormones (ie. you have heart disease, blood clot disorder, etc. Discuss with your doctor first.).
What’s new in birth control?
There’s a new birth control vaginal ring, patch, and progestin-only pill.
The new vaginal ring is Annovera, which carries a new progesterone segesterone and a very low dose of estrogen (13 mcg per day). The benefit of the new progesterone segesterone is that it does not have androgenic side effects like acne, blood lipid effects, hairiness, etc.
This method may not be best for those under 30 years old, however. The concern is that this estrogen level may negatively impact women who are under that age. A pediatric endocrinologist, pediatric adolescent gynecologist, and adolescent medicine doctors at Stanford recommend at least 30 mcg of estrogen for birth control pills, because research has shown that lower levels result in lower bone mineral density.
Annovera is placed intravaginally for 21 days then removed and out of the body for one week (during which time the user will experience a withdrawal bleed). It has not been tested for continuous use (skipping periods).
The cost without insurance is about $2000 and the cost with insurance and under the ACA should be “free” (no copay, no deductible).
You might want to try the one-month ring (NuvaRing, EluRyng) to see if you like a vaginal ring before trying Annovera.
The new birth control patch is called TWIRLA, which contains levonorgestrel and ethinyl estradiol. A woman uses one patch a week for three weeks, and then during the 4th week no patch is needed (during which time, a withdrawal bleed occurs).
Of note: If your BMI is 25-30, it might not work as well. And If your BMI is 30 or greater, the manufacturer does not recommend you use it because:
1. It doesn’t work as well
2. It puts you at higher risk for a blood clot.
The concern about the patch is that previous studies have shown that the risk of developing a blood clot [venous thromboembolism (VTE)] is twice as likely on the patch than on standard birth control pills. This is thought to be due to the fact that the hormone goes through the skin and skips having to go through the stomach.
The benefit of this patch is that it is slightly lower in estrogen (30 mcg vs. the Xulane patch at 35 mcg). However, users will most likely still experience higher levels in the blood than with birth control pills. The major side effect noticed is breast tenderness compared to birth control pills, but this was of similar levels to those on the birth control pills after the 1st month.
There is a also new progesterone-only pill (POP): Slynd. The benefit to this pill is that it has a much more forgiving window of effectiveness. For most POPs, if you are three hours late taking it, you need to abstain from heterosexual intercourse or use a backup for the next few days and use emergency contraception if you have had heterosexual intercourse in the previous three days. However, Slynd has a 24-hour dosing window, like the “regular” birth control pills, which contain estrogen and progesterone. The major drawback of Slynd is cost: $193-$268 per month vs. regular birth control pills at $15 per month or other POPs at $8-$30 per month. Also, the progesterone in Slynd is drospirenone, which is not good for anyone with kidney issues. Generally, I like to make sure the patient can drink eight glasses of water a day because it might have a diuretic effect which may result in headaches if the patient doesn’t drink enough water.
For further information about the birth-control options available, visit Pandia Health.
Dr. Sophia Yen is Co-Founder and CEO of Pandia Health, the only #WomenFounded, #WomenLed, #DoctorLed birth control delivery company.